So, I jokingly referred to getting this at Unbound but I now have questions related to other’s experiences
After the ER visit, in Kansas, I was placed on Elliquis and Toprol XL. The Toprol helped control the HR but I remained in Afib (Toprol is a cardioselective Beta blocker that helps to control rate). I have tried very easy runs but get winded if I try any effort.
One week after the ER visit, I got in to see my cardiologist and he tried pharmacological cardioversion…Flecainide 300mg taken in the office. He asked me to come back later in the day to see if I had converted back to NSR (normal sinus rhythm), but I had not. About two hours after I left his office, I did convert to NSR (I have a Kardia device at home and this is nice for a quick evaluation). I have stayed in NSR except when i try to exercise. I can run about 3 miles, very easy, and not feel any symptoms. Between miles 3 to 4, I can feel the “fluttering” in my chest, and back at the car, the Kardia confirms Afib. Within 1-3 hours, I convert back to NSR.
I told my doc about this and he suggested trying a daily dose of Flecainide to see if this could help keep me in NSR better. When I took the Flecainide 300mg, it gave me a very strange sensation when I was running. I would feel like my heart was not able to keep up enough for my breathing. It was actually a little bit scary to feel that way with such an easy effort, and I did not feel a similar sensation when I was on Toprol only. After I mentioned this, he had me set up to see an electrophysiologist about an ablation.
So, I’m curious about other’s experience with Flecainide? I’m worried I’m not giving it a chance and it may not be as bad on a much lower daily dose (50mg twice daily vs the one time 300mg dose I took). My cardiologist was, of course, not sure how I would respond to a lower daily dose. When I search for “Flecainide” on here, the most recent was from 2020, so I am hoping there are others here with more recent or long term experience.
most of my patients don’t really mind the flec-but most do NOT like beta blockers and how they feel on them…almost all athletic/active patients want to be back in sinus and feel much better.
Getting the heart rhythm right chemically or electrically *(or both) is often needed. Ablation is next level for a more permanent solution.
I’ve written a lot about afib and I think there is additional information in this thread:
Atrial fibrillation as a athlete. (Page 2): Triathlon Forum: Slowtwitch Forums
(my post is on page two third from last)
It’s funny, just recently I was PMing a member here about fib/flutter and the differences etc
When in atrial flutter, the atria are going very fast, fluttering at ~280-300 bpm, but sometimes the actual heart rate is slower because there is slowing through the AV node.
A-FL can go 1:1 on rare occasions and bad things happen–usually fainting, sometimes cardiac arrest–it’s one reason we have the protector AV node which regulates things a bit.
And it is often a ratio like 4/1–top chamber going 280, bottom chamber (ventricle) going like 70 is one example
No one feels the top chamber beating, only if the actual heart is beating fast, which is dependent on the ventricular response-ie how fast the bottom chamber is beating.
Many people go into persistent afib/flutter and most people do feel it as the ventricular rate is USUALLY fast and patients feel palpitations/fluttering from the fast heartbeats.
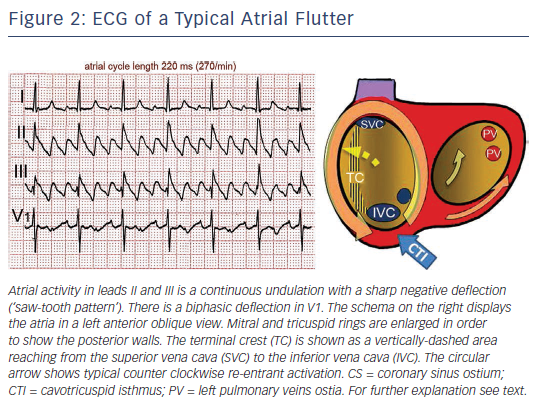
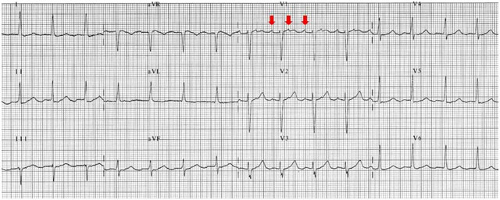
Atrial flutter usually comes in two flavors-typical and atypical. They are distinct on EKG.
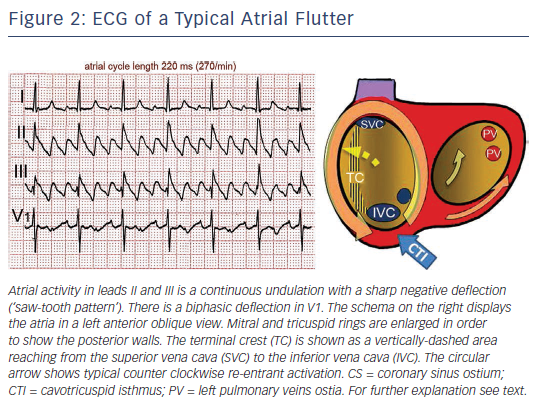
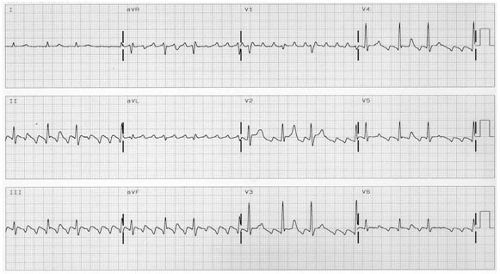
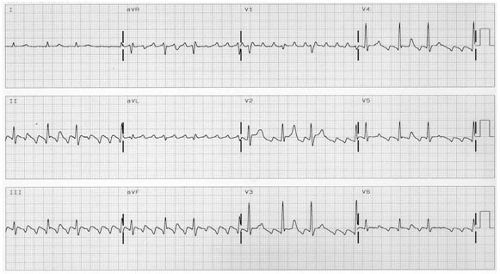
In this example, the ventricular response is controlled (60-100 bpm)
another example-typical ‘sawtooth’ looking atrial flutter waves
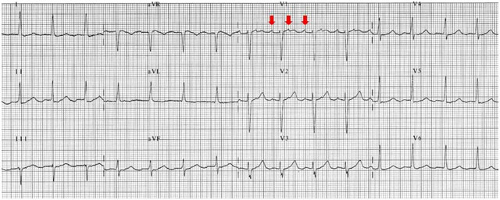
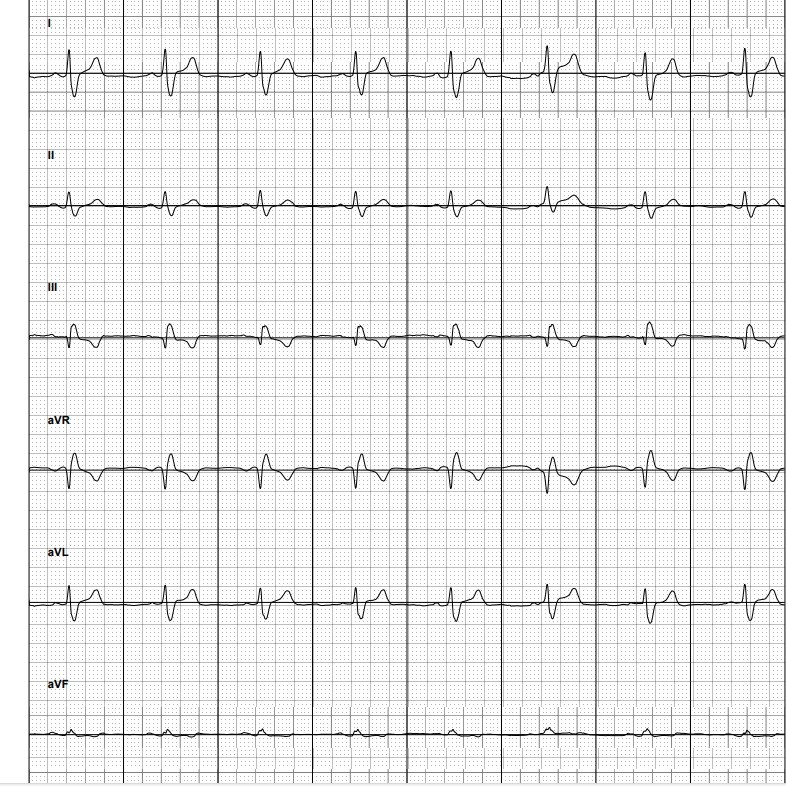
Atypical atrial flutter, aka atrial tachycardia-is a bit harder to see

Saw an electrophysiologist today. He says I appear to be in atrial flutter. I showed him my Kardia readings and even though they read as “normal sinus rhythmâ€, he says there’s still enough irregularities that it’s flutter (and repeat EKG today confirmed this).
So, he wants to do a cardioversion (electrical) to try and get me back to NSR. Hoping to have that done soon. If that does not allow me to stay in NSR then he said an ablation would be in order. I am to continue on the Elliquis
as you can see, atypical flutter can look an awful lot like regular sinus-and it can look very similar both by ekg and on the Kardia -