Here is a little fun game :). Below are my latest numbers from the doc. I am at high-risk for a MI, stroke, and heart valve issues. I discovered this 18 months ago when I went into cardiac arrest due to an MI(you can read about it in my other thread.) So here is the game, take a look at my numbers below, try to identify which one identity’s the risk. Why is this important? Because many people have asked me if there was any testing/data that would have identified my risk prior to my MI. At the time the doctors seemed to tell me “not really, at least not a test we would have performed on you because your risk would have been identified as ‘low’, no further testing needed”… but now I know more and there certainly was something that we missed… something that EVERYONE (in my opinion) should get checked. So here ya go, these are my numbers and data:
Age: 48 (male)
Heart Rate (resting: 38bpm
Blood pressure: 112/61 mmHg
Weight: 172 pounds (typical race weight is 162-165)
Height 5’9"
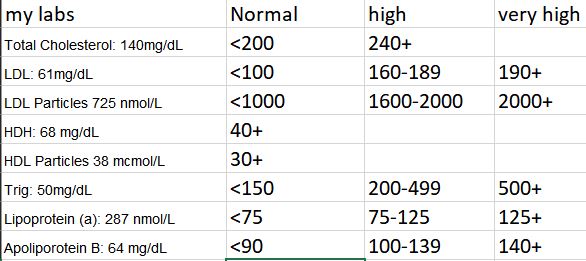
Blood results:
Total Cholesterol: 140mg/dL
LDL: 61mg/dL
LDL Particles 725 nmol/L
HDH: 68 mg/dL
HDL Particles 38 mcmol/L
Trig: 50mg/dL
Lipoprotein (a): 287 nmol/L
Apoliporotein B: 64 mg/dL
ECG Results:
Ventricular Rate (HR): 30BPM (this set off alarms on the machine… opps!)
PR int: 176 ms
QRSD int: 116ms
QT int: 480ms
QTC Int: 339ms
P Axis -22deg
R Axis 43deg
tWave axis 60deg
Echo results:
Ejection factor: 61%
No significant valvular heart disease
Normal flow pattern
Normal left ventricular filling pressure
(I won’t post all the numbers from the echo… but all in the normal range)
History:
Previous heart disease/issues: None (prior to MI/CA in Feb 2021)
Family history of heart disease: None
Medications (prior to MI event) None (now they have me on a ton of stuff)
Other health issues: None
Smoker?: Never.
Alcohol: Some beer and red wine when not race season… but nothing noteworthy.
Diet: 90% vegan, low fat, low sodium, lots of fruits and veggies. (@synthetic will tell you that my diet must be crap because i don’t eat just kale and carrots)
Cardio Activity: Prior to MI in 2021: Competitive amateur triathlete, USAT All-American for 45-49AG, 12-14 hours of training a week, (these days I still train but not as much and not at the same intensity… but still very active.
Okay… So how does this compare to your numbers and lifestyle? And can you figure out why I am at high risk for a MI, stroke, and heart valve issues?